Introduction: Autoimmune thrombotic thrombocytopenic purpura (aTTP) is a severe disease caused by the production of autoantibodies against von Willebrand factor (vWF)-cleaving ADAMTS13 (a disintegrin and metalloproteinase with thrombospondin-1 motifs; 13th member of the family). Without functional ADAMTS13, endothelial cells-derived unusually large vWF (ULVWF) multimers are present and are responsible for platelet clumping in the microvasculature. Plasma exchange (PE) and immunosuppressive therapy with steroids and rituximab are the milestones of the treatment of this disease. Moreover, in 2018, nanobody caplacizumab was approved for the treatment of adult patients with an acute episode of aTTP. Our objective was to retrospectively review the efficacy and safety of the current use of caplacizumab in Spain.
Methods: We collected demographic, clinical, and laboratory data of patients with aTTP who were reported in the TTP Spanish Registry from 15 centres between July 2018 and July 2020. All patients were diagnosed with aTTP because of the presence of microangiopathic hemolytic anemia (MAHA), thrombocytopenia, organ dysfunction, ADAMTS13 activity less than 5% and the presence of ADAMTS13 autoantibodies. Qualitative data are presented as number (frequencies). Quantitative data are presented as mean ± standard deviation (SD) or median (interquartile range -IQR-) when appropriate. A correlation test was performed to determine the linear relationship between number of days since diagnosis to caplacizumab start and number of days since diagnosis to the first day with >150x109/L platelets.
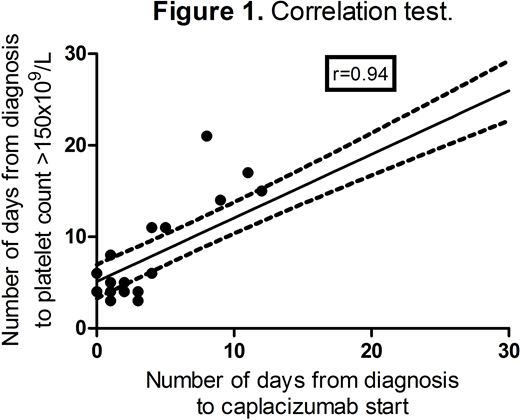
Results: Our series comprises 30 patients: 22 (73%) females and 8 (27%) males with a median age of 45 (IQR: 31-55). At presentation, neurologic abnormalities were seen in 18 (60%) patients, symptoms and signs of anemia were present in 15 (50%) patients, and bleeding was present in 10 (33%) patients. Fever was present in 1 (3%) patient. Laboratory tests showed hemoglobin 92±28 g/L, platelet count 19±16 x109/L, unconjugated bilirubin 2.33±1.76 mg/dL, LDH 1,467±1,428 IU/L, and creatinine 1.0±0.45 mg/dL. Median ADAMTS13 activity was 0 (IQR: 0-0.5) and ADAMTS13 autoantibodies were positive in all cases. After diagnosis, treatment was started with PE and steroids in all patients after a median of 0 days (IQR: 0-0) and patients received a median of 10 PE procedures (IQR: 7-13). Caplacizumab was administered to all patients with a median of 3 (IQR: 1-9) days after diagnosis and it was administered during 36 days (IQR: 31-39). No severe adverse events were reported with the use of caplacizumab. Rituximab was added in 19 (63%) patients after a median of 4 days (IQR: 14-21). Time to platelet normalization (>150x109/L) was 5.5 days (IQR: 4-17) after diagnosis. The longer the delay in administering caplacizumab after diagnosis, the longer the delay in platelet normalization (Pearson's correlation coefficient, r=0.94 (95% CI: 0.86 to 0.98; R2=0.89; p<0.01; figure 1). Clinical remission was achieved in 29 (97%) patients after a median of 8 days (IQR: 4-14). One (3%) patient died because of aTTP complications 11 days after diagnosis. One patient was refractory to PE, steroids, rituximab, caplacizumab, and she achieved clinical remission after receiving vincristine and cyclophosphamide.
Conclusion: Caplacizumab was an efficacious and safe drug to treat adult patients with acute episodes of aTTP. A statistically significant strong positive linear correlation was observed between number of days from diagnosis to caplacizumab start and number of days from diagnosis to the first day with >150x109/L platelets.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal